What Is Uveitis?
What Causes Uveitis?
The specific cause of uveitis often remains unknown in most cases. The word “idiopathic” may often be used to describe this group
Uveitis may be associated with:
| • Systemic inflammatory diseases; |
| • A result of injury to the eye; or |
| • It may be associated with infection caused by virus, bacteria, fungus or a parasite. |
Types Of Uveitis
Uveitis can be of four types, depending upon the location of the inflammation. There are several types of uveitis, defined by the part of the eye where it occurs.
| • Iritis or Anterior Uveitis affects the front of your eye. This is the most common type of uveitis. Iritis usually develops suddenly and is commonly associated with redness, watering, decreased vision, pain in the eye and photophobia or intense discomfort while looking at light. Some types of anterior uveitis can be chronic or recurrent. | 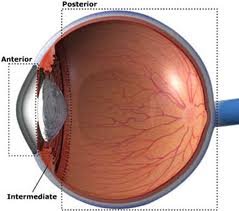 |
| • Pars planitis or Intermediate uveitis affects the middle or intermediate region of the eye. The patient usually sees black spots in front of the eye. There may be loss of vision due to fluid accumulation in the central area of the retina. The disease goes through cycles of getting better, then worse. | |
| • Posterior uveitis affects the back parts of your eye. Posterior uveitis can develop slowly and often lasts for many years. The inflammation may affect the retina, choroid (posterior or back part of the middle layer) or both. The inflammation may be localized at several places, or even widely spread. Patients usually complain of poor vision, or the absence of central or peripheral vision. The eye may appear normal or there may be little inflammation in the front. | |
| • Panuveitis occurs when all layers of the uvea are inflamed. It often causes a distinct blurring of the vision with varying degrees of pain and redness. | |
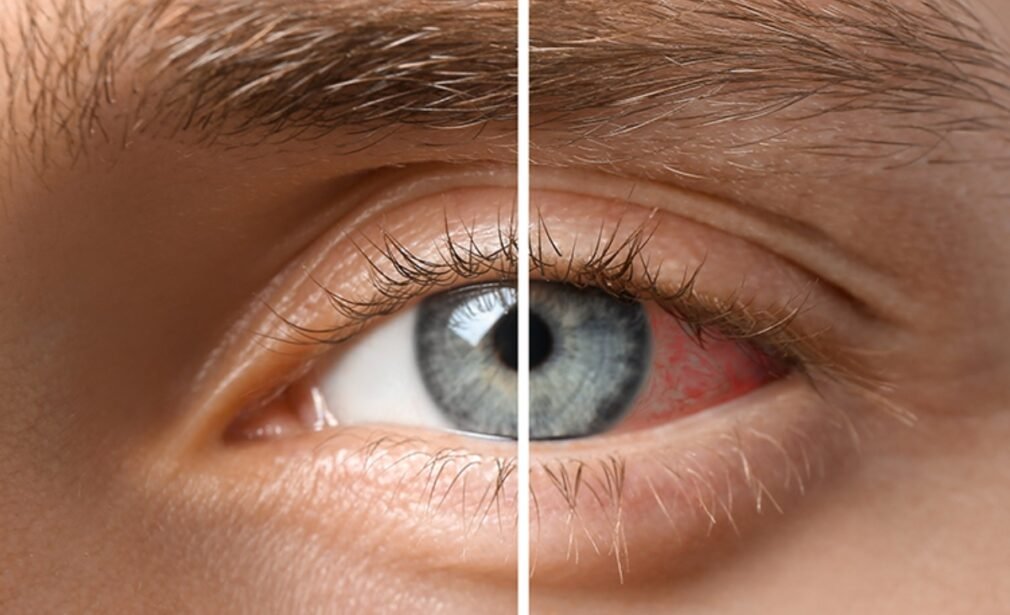
Symptoms of Uveitis
Uveitis may develop suddenly with eye redness and pain, or with a painless blurring of vision. In addition, other symptoms of uveitis may include light sensitivity, blurred vision, decreased vision and floaters. There may also be a whitish area (called a hypopyon) obscuring the lower part of the iris.
Diagnosis of Uveitis
A careful eye examination by an ophthalmologist is extremely important when symptoms occur. Inflammation inside the eye can permanently affect sight or even lead to blindness if it is not treated.
Your ophthalmologist will examine the inside of your eye. He or she may order blood tests, skin tests or X-rays to help make the diagnosis.
Since uveitis can be associated with disease in other parts of the body, your ophthalmologist will want to know about your overall health. He or she may want to consult with your primary care physician or other medical specialists. However, in approximately 40 to 60 percent of cases, no associated disease can be identified.
Uveitis Treatment In Andheri: What We Offer
The treatment of Uveitis aims to achieve the following:
| • Relief of pain and discomfort (where present) |
| • To prevent sight loss due to the disease or its complications |
| • To treat the cause of the disease where possible |
Like the varied nature of uveitis, the treatment of it may differ from case to case quite considerably.
At times patient may be referred to other specialities for confirmation of systemic diseases.
Specific treatment is given for entities like TB or Toxoplasmosis uveitis. Corticosteroids are often the mainstay of treatment to control inflammation. But now we have some other newer drugs like immunosuppressive drugs usually used along with the steroids for immunological causes.
| • If you have a “red eye” that does not clear up quickly, contact your ophthalmologist. |
| • Uveitis is a serious eye condition that may scar the eye. It needs to be treated as soon as possible. Eyedrops, especially corticosteroids and pupil dilators, can reduce inflammation and pain. For more severe inflammation, oral medication or injections may be necessary. |
| • Even though there may not be a permanent cure for Uveitis, each attack can be treated, depending upon the cause, severity and location of the inflammation. The treatment may include eye drops, injections under the eye or oral medication. These drugs have potential side effects, but they are often not serious and their effects are reversible, once treatment is discontinued |
If left untreated, uveitis may lead to:
| • Glaucoma (increased pressure in the eye); |
| • Cataract (clouding of the eye’s natural lens); |
| • Neovascularization (growth of new, abnormal blood vessels); or |
| • Damage to the retina, including retinal detachment, damage to the optic nerve or both. |
It is important to maintain regular follow-up by your treating ophthalmologist in order to monitor medications as well as progression of the disease. Because of the serious complications which may occur as a result of uveitis, an ongoing partnership between patient and ophthalmologist greatly increases long-term success.